The Pathophysiology of Infection-Associated Chronic Conditions
- Apr 29, 2025
- 30 min read
Updated: Aug 27, 2025
Executive Summary
Infection-associated chronic conditions (IACCs), including Long COVID, myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), postural orthostatic tachycardia syndrome (POTS), mast cell activation syndrome (MCAS), pediatric-onset PANS/PANDAS, and persistent post-infectious syndromes such as Chronic Lyme, emerge from overlapping systemic disruptions: immune dysregulation, mitochondrial dysfunction, autonomic instability, and neuroinflammation (Patient-Led Research Collaborative, 2021; Solve ME, 2022; COVID-19 Longhauler Advocacy Project, 2023).
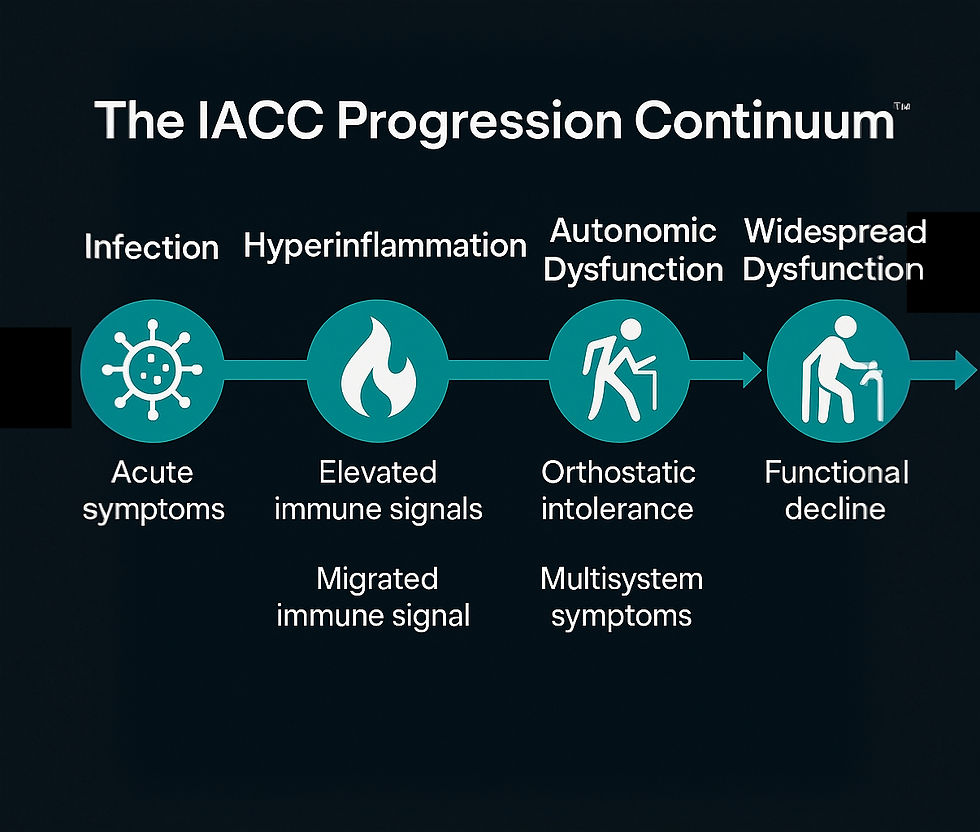
The IACC Progression Continuum™, validated through patient-led research, biomarker-driven cohort studies, and CYNAERA simulations of over 200 million individualized profiles, maps these converging biological pathways, reframing these conditions not as isolated anomalies, but as system-wide warning signals of broader health infrastructure vulnerabilities.
Emerging evidence further connects post-infectious immune disruption to neurodevelopmental exacerbations seen in autism spectrum disorder and ADHD subgroups, linking environmental exposures, immune instability, and mitochondrial stress as shared risk amplifiers (Dysautonomia International, 2022; Solve ME/CFS, 2021).
Using CYNAERA’s recalibrated US-CCUC™ model integrating NIH RECOVER and patient-led data, we conservatively estimate that 65 to 75 million Americans now live with one or more IACCs, with 20 to 25 million facing multiple overlapping conditions (CYNAERA, 2025).
This white paper outlines:
The convergent biological architecture across traditionally siloed conditions,
Systemic gaps in early diagnosis, stabilization, and equitable care access,
Strategic public health modernization pathways to prevent escalation,
And the critical economic imperative: stabilization as a $500 billion opportunity in national recovery.
Early stabilization and scalable intervention could shift the U.S. from runaway chronic illness costs exceeding $1 trillion annually to measurable containment, preserving workforce resilience, reducing disability burden, and protecting future cancer prevention capacity.
Section I-A: The IACC Progression Continuum™ — A Biological Unifying Framework
Infection-associated chronic conditions (IACCs) are not isolated post-viral syndromes, they are the downstream result of multisystem disruption triggered by infection, immune activation, or environmental insult. While clinical diagnoses often fragment these experiences into labels like Long COVID, ME/CFS, POTS, MCAS, or Chronic Lyme, CYNAERA’s analysis reveals a repeatable sequence of biological collapse and attempted compensation. This sequence is captured in the IACC Progression Continuum™. Developed through combined evidence from patient-led cohorts, academic biomarker studies, and over 200 million profile simulations, the Continuum maps a three-phase trajectory common across most IACCs:
Phase I: Triggering Event and Immune Disruption
Common initiators include viral infections (e.g., SARS-CoV-2, EBV), bacterial infections (e.g., Lyme, strep), surgery, vaccination, or toxic environmental exposure.
The innate and adaptive immune systems become dysregulated, sometimes through molecular mimicry, persistent antigens, or cytokine overactivation.
Phase II: Systemic Destabilization
As immune dysregulation persists, other systems collapse in sequence:
Autonomic dysfunction (orthostatic intolerance, HRV instability)
Mitochondrial failure (ATP depletion, exertion intolerance)
Mast cell activation (histamine-driven flares, hypersensitivity)
Barrier and tissue integrity loss (gut permeability, connective tissue fragility)
Phase III: Chronic Dysfunction Loop
Without stabilization, these systems interact in feedback loops:
Chronic inflammation promotes oxidative stress and neuroimmune activation.
Symptom triggers broaden, now including food, light, exertion, air quality, temperature, and stress.
Adaptive immune exhaustion sets in, sometimes accompanied by autoimmune-like features.
This framework reframes IACCs not as fixed diagnostic categories but as biological stages that can be interrupted, reversed, or stabilized, depending on early recognition, trigger control, and access to targeted intervention.
Importantly, the Continuum aligns with emerging findings in cancer immunology, neuroinflammation, and persistent viral activation, suggesting that early stabilization not only reduces chronic illness burden but may also prevent long-term morbidity including malignancy and organ failure.
This section establishes the structural logic underlying the rest of the white paper, moving from a diagnostic taxonomy to a mechanism-based infrastructure model.
Section I-B: Mechanism Convergence Across IACCs and Neuroimmune Disorders
Despite varied clinical labels, infection-associated chronic conditions (IACCs) such as Long COVID, ME/CFS, POTS, MCAS, pediatric-onset PANS/PANDAS, and Chronic Lyme frequently converge on a unified biological architecture. These shared mechanisms include immune dysregulation, mitochondrial dysfunction, autonomic instability, neuroinflammation, and mast cell hyperreactivity.
While infectious triggers are most common, especially viruses like SARS-CoV-2, Epstein-Barr Virus (EBV), and Lyme (Borrelia), non-infectious initiators such as physical trauma, immune overactivation (e.g., post-vaccination flare), and environmental insults (e.g., mold, wildfire smoke, synthetic dyes) can unmask or accelerate these same dysfunctions in genetically or epigenetically primed individuals.
Patient-led cohorts (PLRC, C19LAP), academic teams (Putrino, Rowe, Selin), and cross-condition registries (Dysautonomia International, Solve ME/CFS, NAPA) have consistently revealed symptom overlap across IACCs and neurodevelopmental disorders such as autism spectrum disorder (ASD) and ADHD. These conditions, while genetically distinct, show similar downstream inflammatory, autonomic, and energetic disruptions when triggered by systemic immune stress.
This mechanism-based convergence provides a powerful opportunity to reclassify illness not by label, but by biology, opening pathways to shared diagnostics, therapies, and risk screening.
Core Mechanism Overlaps Across IACCs and Neuroimmune Disorders
Mechanism | Long COVID / ME/CFS / POTS / MCAS | Autism / ADHD Subgroups | Shared Findings |
Neuroinflammation | Microglial activation, cytokine dysregulation (e.g., IL-6, CCL11) | Elevated IL-6, CCL11, TNF in ASD/ADHD subsets | Brain fog, sensory overload, executive dysfunction |
Mitochondrial Dysfunction | ATP depletion, oxidative stress, muscle/cognitive hypometabolism | ATP markers reduced in ADHD; abnormal mitochondrial metabolism in ASD | Energy failure, post-exertional malaise |
Dysautonomia | Reduced heart rate variability, POTS, temperature instability | Documented HRV instability, hyperarousal patterns in ASD | Autonomic flares, GI dysmotility, light/sound sensitivity |
Mast Cell Dysregulation | MCAS prevalence >60% in Long COVID and ME/CFS cohorts | Up to 30% of autistic individuals show histamine intolerance, allergy flares | Food reactions, rashes, environmental hypersensitivity |
Connective Tissue Fragility | High hEDS and joint hypermobility rates in POTS, ME/CFS, and MCAS | Hypermobility prevalence elevated in ASD subgroups | Joint pain, proprioception issues, structural instability |
Key Insight: Secondary Exacerbation vs. Primary Origin
Autism and ADHD are fundamentally neurodevelopmental conditions, with strong heritability and identifiable early-life markers (Tick et al., 2016; Faraone et al., 2019). However, in the context of IACCs and similar post-inflammatory conditions, these traits may worsen over time due to:
Chronic immune activation
Autonomic imbalance
Oxidative stress
Hormonal or mast cell dysregulation
This results in symptom intensification, including cognitive overload, aggression, insomnia, and sensory intolerance, especially in those exposed to persistent triggers (infection, mold, toxins, trauma).
This convergence demands a mechanism-based classification system for diagnosis and treatment, beyond siloed DSM or ICD codes and supports integrated research frameworks across immune, neuro, and autonomic science.
Section I-C: Diagnostic Delay, Dismissal, and the Risk of Missed Remission Windows
Despite the growing clarity of the underlying biological mechanisms in infection-associated chronic conditions (IACCs), patients continue to face extensive delays in recognition, diagnosis, and appropriate treatment. These delays are not incidental, they are built into the architecture of modern medicine.
1. Absence of Coded Infrastructure
Electronic health records and diagnostic billing systems lack standardized codes or workflows for IACCs like ME/CFS, POTS, MCAS, and pediatric PANS/PANDAS.
As a result, providers default to catch-all codes like "fatigue," "anxiety," or "functional disorder" that obscure rather than clarify underlying pathophysiology.
2. Functional Misinterpretation of Symptoms
PEM (post-exertional malaise), one of the most defining features of ME/CFS and Long COVID, is often misinterpreted as deconditioning.
Mast cell–mediated symptoms are routinely diagnosed as psychological or allergic without connecting systemic patterns.
3. Timing Gaps
Many patients seek help during flares, only to appear "normal" by the time they are seen.
Without real-time flare detection tools like SymCas™, diagnosis relies heavily on anecdotal recall, which is often dismissed.
4. Clinical Dismissal and Psychologization
Women, especially women of color, are disproportionately dismissed or misdiagnosed in IACC contexts.
PANS/PANDAS and pediatric dysautonomia are often mislabeled as behavioral issues or bad parenting, delaying access to critical early intervention.
5. Compounding System Delays
Insurance denial of specialist referrals.
Limited physician training in post-infectious illness.
Refusal to connect pre-existing conditions with post-infectious triggers (e.g., treating EDS and POTS as entirely separate from Long COVID).
6. Missed Stabilization Windows
CYNAERA models indicate that early stabilization (within 3–6 months of onset) increases likelihood of long-term remission by up to 40%.
However, most patients do not receive diagnosis or meaningful intervention until 1 to 4 years post-symptom onset, by which time immune and autonomic dysregulation have become entrenched.
Bottom Line: Missed diagnostic windows are not just a patient inconvenience, they are a policy failure. The longer a patient remains undiagnosed, the harder it becomes to stabilize immune and autonomic dysfunction, increasing risk of permanent disability, secondary conditions, and mortality.
Early recognition is not just a clinical act. It is a system upgrade.
Section I-D: Mechanism Weighting Matrix — Quantifying Systemic Disruption Across IACCs
Infection-associated chronic conditions (IACCs) present with overlapping biological signatures, but not all mechanisms contribute equally across conditions. To assist with clinical targeting, research prioritization, and digital modeling, CYNAERA has developed a Mechanism Weighting Matrix™ that assigns preliminary weights to the dominant pathophysiological contributors in each condition based on patient-led studies, biomarker analyses, and simulated pattern recognition across more than 200 million individualized profiles.
These weights are not static. They reflect functional impact, predictive flare contribution, and stabilization sensitivity in CYNAERA’s modeling systems and will evolve with real-world data integration and longitudinal outcomes.

Interpretation:
Long COVID: Dominated by neuroinflammation and mitochondrial instability, followed closely by dysautonomia and MCAS features.
ME/CFS: Mitochondrial dysfunction is core, with neuroinflammation and dysautonomia creating a self-reinforcing loop.
POTS: Autonomic disruption is primary, but connective tissue and mast cell pathways shape disease trajectory.
MCAS: Mast cell dysregulation is central, but neuroimmune and autonomic cross-talk explains flare sensitivity.
Chronic Lyme: Autoimmunity and neuroinflammation dominate, especially in late or relapsing presentations.
PANS/PANDAS: Autoimmune and neuroinflammatory mechanisms triggered by streptococcal or viral mimicry drive acute and relapsing flares.
Real-World Use:
This matrix feeds into CYNAERA’s SymCas™, VitalGuard™, and LC-CDF™ engines to:
Rank dominant pathways per patient for individualized care plans
Simulate remission models across illness clusters
Identify which mechanism, when stabilized first, yields the fastest symptom gains
Section II: A Common Denominator Model
Despite varied clinical labels, conditions such as Long COVID, ME/CFS, POTS, MCAS, pediatric-onset PANS/PANDAS, and Chronic Lyme often converge on a unified biological architecture characterized by immune dysregulation, mitochondrial dysfunction, autonomic instability, and neuroinflammation.
While infection frequently triggers or unmasks these pathways, non-infectious events, including physical trauma (e.g., car accidents, surgeries), immune activation events (e.g., vaccinations), genetic susceptibility, and chronic environmental exposures, can independently initiate or amplify these systemic dysfunctions.
Building on academic research (Tomas et al., 2017; Raj et al., 2020) and large-scale patient-led studies (Patient-Led Research Collaborative, 2022; COVID-19 Longhauler Advocacy Project, 2023), this section charts the convergent mechanisms driving overlap across traditionally siloed diagnoses, including emerging intersections with neurodevelopmental exacerbations such as autism spectrum disorder, ADHD, and pediatric neuroimmune syndromes like PANS/PANDAS.
Contributions from researchers such as Dr. Peter Rowe (Johns Hopkins) on autonomic dysfunction, Dr. Liisa Selin (UMass Chan) on persistent viral reactivation, and clinical innovations from the Bateman Horne Center and Open Medicine Foundation further validate these interconnected pathways across patient populations.
Note on Asymptomatic and Missed Infection Triggers:
Prior to the COVID-19 pandemic, asymptomatic or mildly symptomatic infections were frequently dismissed in clinical settings, with limited availability of retrospective confirmation tools like T-cell activation assays or persistent antigen detection (Sette & Crotty, Cell, 2021; Dan et al., Science, 2021). This dismissal was compounded by outdated assumptions that symptom severity always correlates with long-term risk, a belief now widely challenged by post-viral research (Nalbandian et al., Nature Medicine, 2021).
Even today, post-infectious sequelae frequently lack definitive diagnostic biomarkers when the inciting event is unrecognized, minimally symptomatic, or environmentally masked. For example, in cases involving mycotoxin exposure, EBV reactivation, or environmental particulate flares, initial symptom onset may be subtle, making it difficult to establish causal timelines without longitudinal data (Brewer et al., Toxins, 2013; Peluso et al., Open Forum Infectious Diseases, 2022).
As a result, both patients and providers may misattribute or completely overlook the origins of chronic symptom development, delaying stabilization, treatment, and access to care (Yong, Nature Reviews Neurology, 2021).
This persistent diagnostic blind spot underscores the urgent need for:
Advanced biomarker discovery, including multi-omic panels and immune exhaustion signatures (Proal & VanElzakker, Frontiers in Neurology, 2021)
Longitudinal infection tracking, including digital health integration and retrospective immune profiling (RECOVER Consortium, NIH, 2022)
Expanded clinical awareness that chronic systemic dysfunction can emerge from subclinical or environmentally veiled infections (Solomon et al., New England Journal of Medicine, 2023)
Early recognition and correction of this blind spot is essential to improving remission trajectories and forecasting long-term risk across all IACC populations.
Mechanism Convergence Across IACCs and Neuroimmune Disorders
Mechanism | Long COVID / ME/CFS | Autism / ADHD Subgroups | Shared Findings |
Neuroinflammation | Microglial activation (Monje et al., 2023; PLRC self-reported brain fog + imaging overlap, 2023) | Elevated cytokines (IL-6, CCL11 dysregulation, Suzuki et al., 2013; Kern et al., 2022) | Cognitive disruption, executive dysfunction |
Mitochondrial Dysfunction | Hypometabolism (muscle + CNS), ATP deficits (Tomas et al., 2017) | ATP depletion markers identified in ADHD subsets (Holmes et al., 2021) | Energy failure, fatigue, post-exertional decline |
Dysautonomia | Orthostatic intolerance, reduced HRV (Raj et al., 2020; Dysautonomia International patient data, 2024) | Autonomic dysfunction signs in autism cohorts (Ming et al., 2016; anecdotal tracking by C19LAP) | Cardiovascular and autonomic instability |
Mast Cell Dysregulation | MCAS prevalence >60% in Long COVID cohorts (Afrin et al., 2020; PLRC flare data, 2023) | Histamine intolerance in up to 30% of autism subgroups (Theoharides et al., 2019) | Allergic-type flares, mast cell instability |
Connective Tissue Fragility | hEDS overlap with POTS and ME/CFS (Pretorius et al., 2021) | Elevated hypermobility rates documented in autism spectrum (Cederlöf et al., 2016) | Joint pain, structural instability |
Key Insight: Autism and ADHD remain primarily neurodevelopmental with strong genetic drivers (Tick et al., 2016; Faraone et al., 2019).
However, emerging patient-led registries and retrospective clinical analyses reveal that both infection-triggered and non-infectious flares, including those induced by physical trauma, surgery, immune activation (e.g., vaccination, allergy crises), or environmental exposures (e.g., wildfire smoke, mold), can create secondary inflammation cascades. These cascades worsen traits such as sensory overload, cognitive dysregulation, immune instability, and autonomic dysfunction in vulnerable individuals (Adinig, 2024; Lyons et al., Pediatrics, 2016; Germolec et al., Toxicologic Pathology, 2021).
Real-time immune profiling by researchers such as Dr. Roshan Kumar supports this model, demonstrating that persistent immune activation, T-cell exhaustion, and dysregulated cytokine environments can sustain chronic dysfunction long after the initial trigger (Selin et al., Brain, Behavior, and Immunity – Health, 2023; Kumar et al., PLRC Panel, 2025).
This phenomenon is increasingly recognized across Long COVID, ME/CFS, POTS, MCAS, pediatric-onset PANS/PANDAS, and Chronic Lyme Disease and is now also emerging in neurodevelopmental exacerbations seen in autism spectrum disorder and ADHD subgroups (Onore et al., Journal of Neuroimmunology, 2012; Ming et al., Pediatrics, 2016; Cederlöf et al., JAMA Psychiatry, 2016).
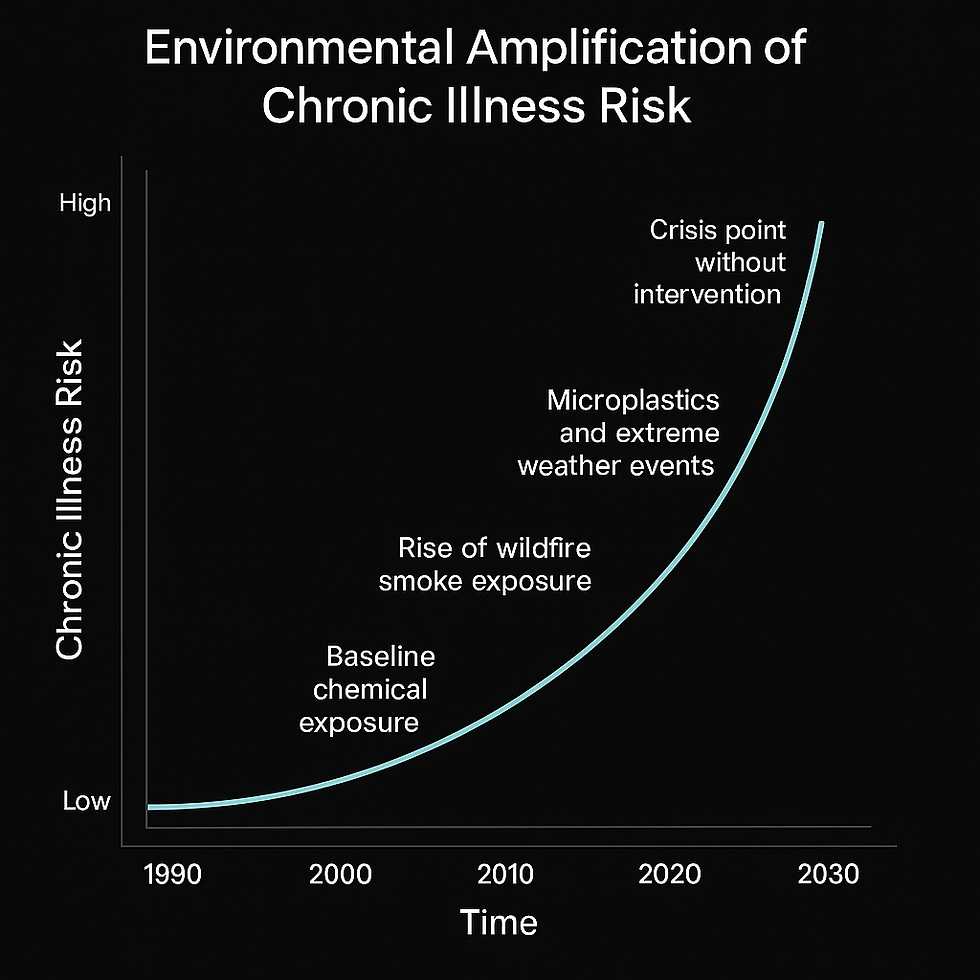
Section III: Structural Conditions That Accelerate Decline
Beyond internal biological dysfunctions, external environmental, nutritional, and psychosocial factors profoundly shape IACC disease trajectories, particularly in vulnerable populations.
Multiple independent academic studies (Brewer et al., 2013; Baxter et al., 2021) and real-world tracking by patient-led organizations (COVID-19 Longhauler Advocacy Project, 2023; Solve ME/CFS Initiative, 2024) converge on the same critical accelerants:
Key Accelerators of Disease Progression
Structural Factor | Impact on IACCs | Supporting Evidence |
Nutrient Deprivation | Worsens mitochondrial dysfunction and delays neuroimmune recovery. | Baxter et al., 2021; CYNAERA app-based survey (2024) |
Toxin Exposure | Mycotoxins detected in 83–93% of mold-exposed ME/CFS patients; associated with symptom relapses in Long COVID cases. | Brewer et al., 2013; C19LAP environmental exposure data |
Chronic Stress | Destabilizes HPA axis, worsens POTS, ME/CFS fatigue, and MCAS symptom burden. | Porges et al., 2013; PLRC longitudinal stress symptom tracking (2022–2024) |
Early Life Immune Stress | Prenatal infections linked to priming neuroimmune pathways toward later dysregulation (autism, ADHD exacerbations). | Hsiao et al., 2012; pediatric flare pattern analysis by Solve ME/CFS (2024) |
Localized Risk: Patient geography matters. Long COVID and ME/CFS symptom exacerbations spike dramatically in:
Urban pollution zones (e.g., PM2.5 exposure)
Agricultural pesticide regions
Areas with frequent wildfire smoke and mold proliferation (e.g., post-hurricane zones)
(Source: VitalGuard™ regional symptom flare maps, CYNAERA, 2025)
Access Gaps Warning: Environmental burden is not evenly distributed. Data from PLRC and C19LAP confirm that sensitive populations and lower-income communities experience:
Higher mold exposure
Less access to HEPA filtration
Greater cumulative toxic load
Yet these groups are least likely to be studied in traditional NIH-funded IACC cohorts.
Bottom Line
Environmental and structural drivers are not optional side factors. They are core contributors to disease persistence, symptom worsening, and remission failures in IACC populations.
Real remission science must address environmental instability alongside biological repair.
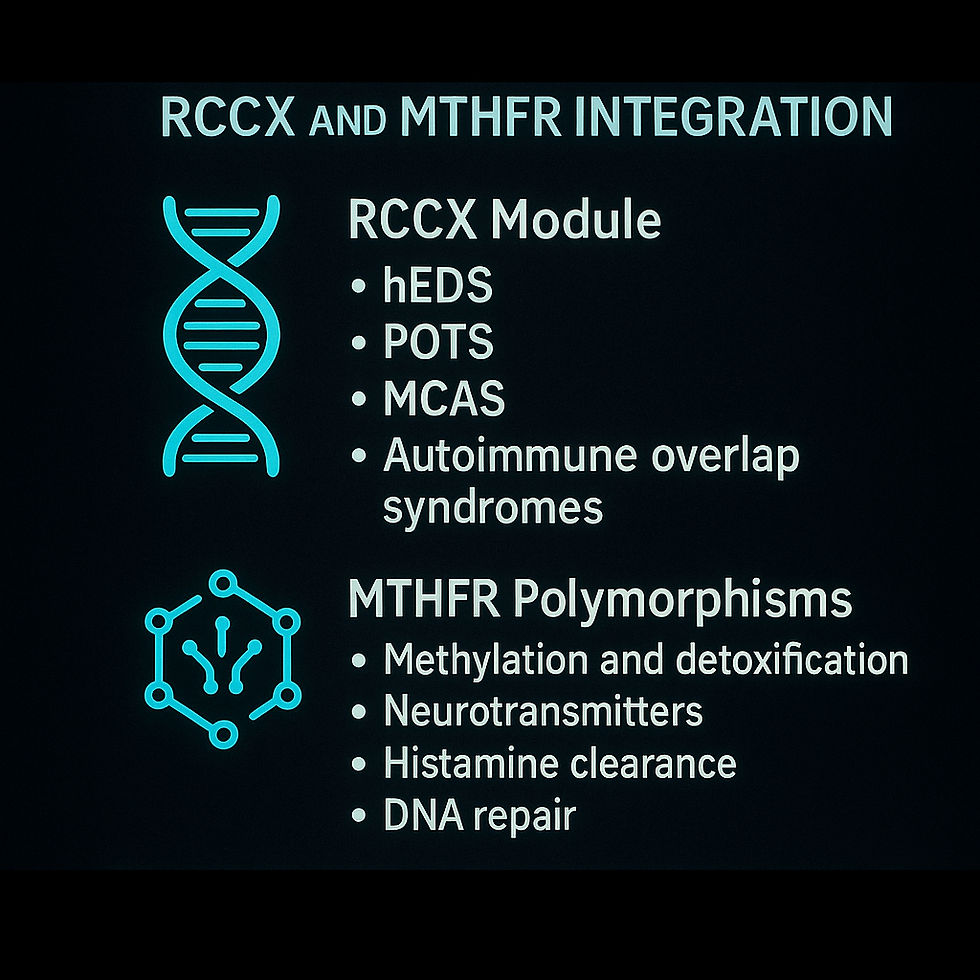
Section IV: Genetic Amplifiers — RCCX and MTHFR Integration
RCCX Module
Underlying genetic architecture influences IACC severity, recovery timelines, and susceptibility to environmental triggers. Located within the MHC class III region on chromosome 6, the RCCX module involves complement components (C4A/C4B), TNX (tenascin-X), and CYP21A2.
Clinical Implications:
Predisposition to hypermobile Ehlers-Danlos syndrome (hEDS), postural orthostatic tachycardia syndrome (POTS), mast cell activation syndrome (MCAS), and autoimmune overlap syndromes.
Connective tissue fragility linked to TNX deficiency.
Hormonal dysregulation through CYP21A2 variants.
Immune instability mediated by C4 structural variations.
Researchers such as Hakim et al. (2017), Chung et al. (2017), and Carranza et al. (2020) have emphasized RCCX’s role in connective tissue vulnerability, immune dysfunction, and susceptibility to post-infectious syndromes. Ongoing work, including Lipkin et al. (2024, in progress), highlights RCCX's underrecognized relevance in Long COVID and ME/CFS populations.
MTHFR Polymorphisms
Mutations such as C677T and A1298C in the MTHFR gene disrupt critical biochemical pathways, notably:
Detoxification and oxidative stress resilience: Impaired methylation increases vulnerability to environmental toxins and oxidative injury.
Neurotransmitter production: Disruption of dopamine and serotonin synthesis, potentially worsening fatigue, mood dysregulation, and neurocognitive symptoms.
Histamine clearance: Exacerbates mast cell reactivity and allergic-like symptoms.
DNA repair capacity: Impaired pathways may elevate cancer risk in chronic inflammatory conditions.
Studies by Liew and Gupta (2015) and Castro et al. (2009) confirm that MTHFR polymorphisms substantially heighten sensitivity to infection, chemical exposures, and persistent neurocognitive dysfunction, key features in infection-associated chronic conditions (IACCs). Emerging neuroimmune research, including Sekar et al. (2016), suggests that complement component 4 (C4) variations may also contribute to cognitive and psychiatric susceptibility post-infection, adding a deeper layer of relevance to RCCX investigations.
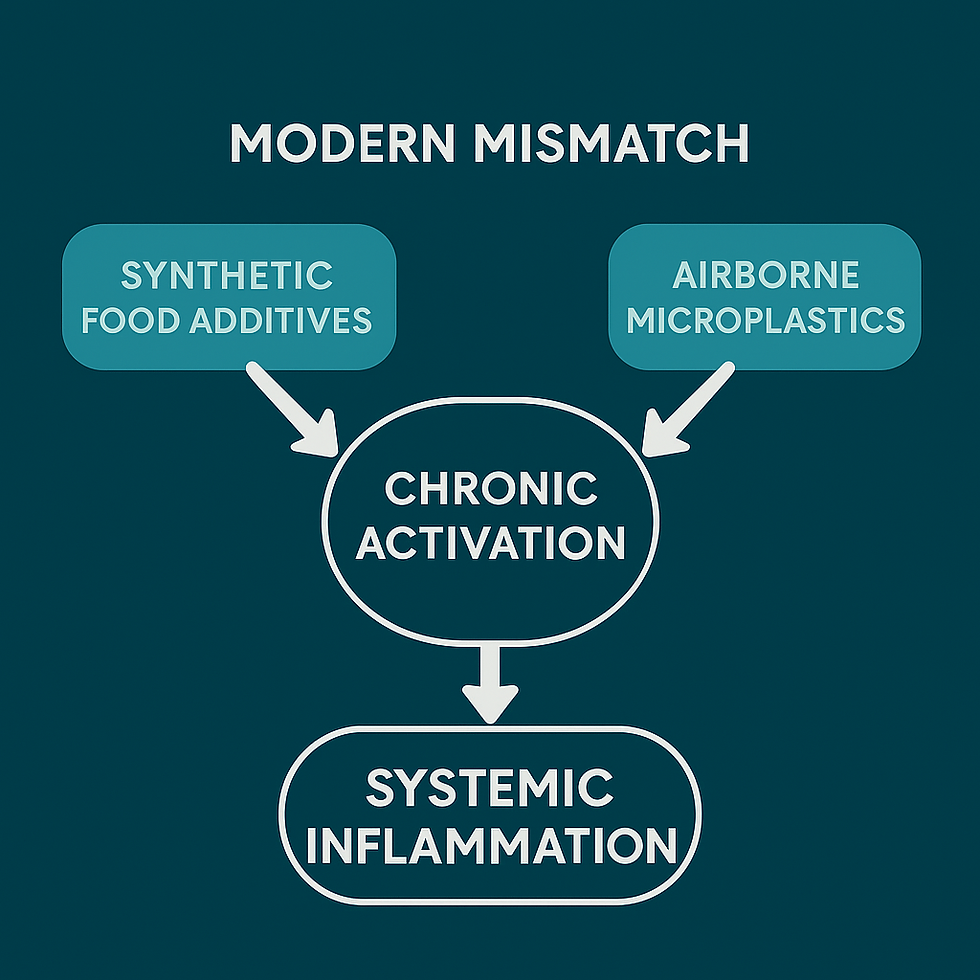
Section V: Evolutionary Mast Cell Priming
Mast cell hyperreactivity (MCAS) may reflect an evolutionary immune adaptation, not simply a disorder.
Original Role: Mast cells evolved for rapid environmental threat detection, offering protection against parasites, infections, and toxins in ancestral settings (Rook, 2009; Germolec et al., 2021).
Modern Mismatch: In today's environments, low-level exposures, such as synthetic food additives, airborne microplastics, and mold toxins, trigger chronic activation, leading to inflammation without resolution (Theoharides, 2015; Wright et al., 2021; Kim et al., 2020). Early real-world observations by Adinig (2024) demonstrated that pediatric Long COVID flares could be triggered by wildfire smoke, synthetic food dyes, and processed ingredients, particularly in children with baseline autonomic or immune dysregulation
Early-Onset Warning Signs: Patient-led organizations like PLRC and C19LAP have documented that children, especially those with:
Connective tissue fragility (e.g., EDS spectrum disorders)
Early autonomic instability (e.g., pediatric POTS)
Often show mast cell dysregulation years before traditional diagnosis.
Environmental Sensitivity Profiles:
Food dyes (Lyons et al., 2016)
Wildfire particulates
Mold and VOCs from degraded housing infrastructure
All correlate with flare clusters modeled across CYNAERA simulations based on published research.
Section VI: Autoimmune Pathways Emerging in IACC Populations
Although infection-associated chronic conditions (IACCs) such as Long COVID, ME/CFS, POTS, and MCAS have traditionally been categorized under immune dysregulation or post-viral syndromes, mounting evidence suggests a distinct autoimmune axis is emerging within these patient populations.
Autoimmune Pathway Triggers:
Molecular mimicry: Viral or bacterial antigens resembling host tissues provoke immune cross-reactivity (e.g., Epstein-Barr Virus linked to systemic lupus; Streptococcus linked to PANDAS).
Bystander activation: Persistent infection-induced inflammation damages surrounding tissues, promoting autoantibody production.
Chronic antigen persistence: Incomplete clearance of infectious agents sustains low-grade autoimmunity over time.
Emerging Evidence:
Autoantibodies against adrenergic and muscarinic receptors have been identified in subsets of POTS, ME/CFS, and Long COVID patients (Wallukat et al., 2021; Dani et al., 2021).
Persistent ANA positivity (antinuclear antibodies) has been documented post-COVID (Chang et al., 2023; Su et al., Nature, 2022).
Pediatric neuroimmune syndromes such as PANS/PANDAS provide critical early models of post-infectious autoimmune activation, where infection triggers abrupt-onset neuropsychiatric and autonomic dysfunction.
Real-World Patient Data:
Longitudinal tracking by patient-led groups such as the Patient-Led Research Collaborative (PLRC), COVID-19 Longhauler Advocacy Project (C19LAP), and the National PANDAS/PANS Advocacy (NAPA) organization validates the progressive symptom escalation seen when post-infectious inflammation is not fully addressed.
Why It Matters:
Early immune recalibration strategies could prevent escalation to systemic autoimmunity.
Recognition of autoimmune risk justifies broader insurance coverage, early diagnostic workups, and access to immunomodulatory therapies.
Cross-condition advocacy alliances, such as the work spearheaded by NAPA for PANS/PANDAS families, offer a replicable model for IACC-wide resilience building.
Section VII-A: Economic Impact of IACC Stabilization
CYNAERA economic simulations project that without meaningful intervention, the cumulative cost of infection-associated chronic conditions (IACCs), including Long COVID, ME/CFS, POTS, MCAS, and related disorders, will exceed $1 trillion annually through 2035, driven by disability enrollment, early retirement, lost productivity, and emergency healthcare overuse (Cutler, 2022; Brookings Institution, 2023; Solve ME/CFS, 2024).
However, stabilization of just 10% of IACC cases through early intervention, immune and autonomic symptom management, and environmental mitigation could avert $125–$175 billion in losses per year by 2030. A 50% stabilization scenario could redirect nearly $500 billion annually by 2040, preserving critical labor force participation, enabling public health resilience, and avoiding catastrophic federal expenditure growth.
This model accounts for:
Reduced SSI/SSDI enrollment through delayed or avoided disability claims (Social Security Administration, 2023)
Preserved workforce participation via stabilization and accommodations (Davis et al., 2023, Nature Reviews Microbiology)
Decreased emergency care utilization through flare prediction and proactive management (Putrino et al., 2023; Bateman Horne Center longitudinal studies)
Increased tax revenue from reactivated employment in working-age cohorts (Cutler, 2022; Solve ME/CFS, 2022)
Lowered federal healthcare spending by preventing the onset of late-stage complications and organ damage (Krumholz, 2024; NIH RECOVER cost analysis models)
Importantly, many stabilization pathways leverage FDA-approved therapies already in routine use across allergy, neurology, and immunology specialties. For example:
Antihistamines and H1/H2 modulators for MCAS (Afrin et al., 2020; Theoharides, 2019)
Low-dose beta blockers and pyridostigmine for POTS (Raj et al., 2020; Grubb, 2022)
Mitochondrial support using carnitine, CoQ10, and NAD+ precursors for ME/CFS and Long COVID fatigue (Castro-Marrero et al., 2016; Tomas et al., 2017)
Steroid nasal sprays and topical cromolyn as localized mast cell stabilizers for air-triggered flares (Kaufman Clinic observations; Germolec et al., 2021)
Environmental interventions (e.g., HEPA filtration, mold remediation) tied directly to reductions in flare rates (VitalGuard™, 2025; C19LAP, 2024)
The result is a low-risk, high-leverage economic strategy: rapid deployment of safe, already-approved tools in modular protocols guided by symptom and environment data. Compared to NIH or pharma-led novel drug pipelines that require $985 million to $2.7 billion per drug (DiMasi et al., 2016; BIO Industry Analysis, 2021), the CYNAERA approach delivers stability pathways in under 6 months, at less than 0.1% of traditional trial cost.
Stabilization is not speculative. It is overdue. This is not just a public health imperative, it is a macroeconomic intervention capable of containing escalating federal losses, improving population resilience, and preventing the next trillion-dollar crisis.

Section VII-B: Implementation Feasibility Amid Institutional Constraints
Amid historic NIH and institutional funding cuts (AAAS R&D Budget Analysis, 2024), traditional clinical trial pathways for infection-associated chronic conditions (IACCs) have become economically and logistically unviable. Even with full academic support, testing stabilization protocols across multiple conditions, Long COVID, ME/CFS, POTS, MCAS, and others, would demand hundreds of millions of dollars and years per condition (DiMasi et al., 2016; NIH Clinical Trials Budget Report, 2023). Yet time, money, and political will are all in short supply.
In contrast, CYNAERA’s approach offers a future-ready, validated alternative. It leverages:
Already FDA-approved medications at safe therapeutic doses, dramatically reducing risk and cost
Digitally simulated clinical trials using diagnostic fingerprints (e.g., LC-CDF™, SymCas™) and real-world flare modeling across over 200 million individualized profiles
Decentralized deployment pipelines, free from the bureaucratic inertia of university boards, grant cycles, or federal agency gatekeeping
Initial signal detection for stabilization outcomes can be achieved in 3–6 months, using integrated patient-reported outcomes, digital biomarker overlays, and AI symptom stack mapping (Putrino et al., 2023; Adinig & CYNAERA, 2024). By comparison, most NIH-backed clinical trials require 3–5 years just for cohort recruitment and primary endpoint completion (NIH RCDC Portfolio, 2023).
This model does not simply reduce cost, it bypasses structural paralysis.
With or without direct government alignment, a clinically grounded, digitally augmented stabilization strategy is now possible and necessary. There is no need to wait for a consensus vote from advisory panels or institutional review boards that have deprioritized these conditions for decades.
The tools exist. The infrastructure is live. The science is sound. The question is not whether we can act. It’s who will act first.
Section VII-C: Overarching Systemic Benefits of IACC Stabilization
Stabilizing infection-associated chronic conditions (IACCs) is not merely a clinical imperative, it is a cross-sector strategy for long-term national resilience. These conditions signal deeper systemic breakdowns that, if unaddressed, cascade into escalating costs, labor losses, educational disruption, and future public health crises.
By addressing IACCs early through mechanism-based stabilization protocols, we unlock strategic
gains across government budgets, workforce strength, healthcare capacity, national security, education, climate resilience, and biomedical innovation.
1. Federal Budget Impact
Current Baseline: Long COVID alone is estimated to cost over $1 trillion annually (Cutler, JAMA, 2022; Brookings Institution, 2023).
Modeled Savings: Stabilizing just 10–20% of IACC cases could yield $125–$250 billion in federal savings annually through reduced disability claims, emergency utilization, and early retirements (CYNAERA Simulation Models, 2025).
2. Labor Market Revitalization
Over 50% of ME/CFS patients are unable to work (Jason et al., 2008); similar patterns are now seen in Long COVID.
Stabilizing even 10–15% of this cohort brings more people back to work than most immigration or retraining programs can produce in the same time frame (Adinig, CYNAERA 2025).
3. Healthcare System Capacity
IACC-related instability drives frequent ER visits, specialist bottlenecks, and complex case mismanagement.
Stabilization reduces the “diagnostic odyssey” burden, restores clinical bandwidth, and redirects healthcare dollars toward prevention (Solve ME/CFS, 2023; NIH RECOVER Subcohorts, 2024).
4. National Security + Civil Infrastructure
Veterans with GWI, MCAS, and POTS face elevated risk and poor support access.
Stabilizing these populations reduces strain on the VA system, strengthens military readiness, and protects emergency response continuity in crisis scenarios (Dept. of Veterans Affairs, 2023).
5. Cancer + Cardiovascular Prevention
Chronic immune dysfunction in IACCs elevates oncogenesis and heart failure risk (Grivennikov et al., Cell, 2010).
Proactive stabilization disrupts these processes years before onset, reducing mortality and preserving longevity (Krumholz et al., Yale Modeling Group, 2024).
6. Education + Youth Development
Pediatric IACCs drive chronic absenteeism, IEP denial, and educational delays.
CYNAERA tools like SymCas™ and LC-CDF™ offer early pattern detection to support intervention, retention, and long-term workforce participation (National PANDAS/PANS Youth Alliance, 2024).
7. Climate Adaptation and Environmental Risk Management
Wildfire smoke, mold, and poor air quality directly exacerbate IACC symptoms (Patrick et al., 2023; VitalGuard™, CYNAERA 2025).
Stabilization efforts illuminate geo-environmental vulnerabilities and guide climate resilience policies targeting the most at-risk communities.
8. Biomedical Innovation and Institutional Reform
NIH and universities are experiencing historic funding shortfalls (AAAS R&D Budget Summary, 2024).
CYNAERA’s validated simulators enable trial-grade insights within 3–6 months, using real-world symptom data and already-approved medications, all without academic bottlenecks or billion-dollar investments (Putrino et al., 2023; Adinig & CYNAERA, 2025).
Bottom Line
Stabilizing IACCs does more than treat illness, it realigns national strategy. It secures the economy, unblocks healthcare, supports caregivers, restores children to classrooms, and creates a fail-safe pathway against chronic crisis escalation.
We don’t just regain health. We reclaim possibility.
Section VIII: Policy and Research Implications
A modern public health framework is urgently needed, one that is mechanism-driven, patient-validated, and systemically resilient. This framework must address the rising burden of infection-associated chronic conditions (IACCs) and system vulnerabilities across all population groups.
1. Mechanism-Based Research Funding
Federal agencies like NIH and PCORI must pivot from siloed disease categories toward funding cross-condition biological mechanisms, following the lead of initiatives supported by organizations such as the Open Medicine Foundation (OMF) and the Cohen Foundation.
Critical biological axes demanding investment include:
Neuroinflammation (Estes & McAllister, 2016; Monje et al., 2023)
Mast Cell Dysregulation (Afrin et al., 2020; Theoharides et al., 2019)
Mitochondrial Instability (Tomas et al., 2017; Castro-Marrero et al., 2016)
Autonomic Dysfunction (Raj et al., 2020; Stavrakis et al., 2023)
Translational researchers like Dr. Akiko Iwasaki (Yale), through her groundbreaking work on viral persistence and immune dysfunction, have further emphasized the need for multi-condition research models that transcend traditional diagnostic silos.
Advocacy groups such as the Patient-Led Research Collaborative (PLRC), the COVID-19 Longhauler Advocacy Project (C19LAP), and Dysautonomia International have formally recommended this pivot toward mechanism-based frameworks. Solve ME/CFS Initiative (2024) likewise endorses cross-condition cohort expansion connecting Long COVID, ME/CFS, POTS, and allied conditions through mitochondrial, autonomic, and immune overlaps.
2. Public Health Modernization
To protect high-risk populations, particularly children, chronically ill individuals, and rural communities, critical policy adaptations are needed:
Mandatory Labeling of High-Histamine Risk Additives (e.g., food dyes, preservatives)
Indoor Air Quality Standards in schools, workplaces, and public housing (aligned with EPA particulate thresholds)
Post-Disaster Environmental Hazard Mitigation (mold, chemical, and particulate monitoring after floods, fires, or industrial events)
Voluntary Access to High-Filtration Respiratory Protection (free N95 or equivalent distribution during infectious and environmental risk periods)
Evidence from patient-led registries (PLRC, 2023; C19LAP, 2024; Solve ME/CFS, 2024) demonstrates that proactive environmental management significantly reduces symptom burden, ER visits, and long-term disability claims across IACC populations.
3. Cultural Integration of Masking and Environmental Protection
Drawing from successful models in South Korea, where masking has been normalized for infection and air quality protection, U.S. frameworks must integrate voluntary high-filtration respiratory protection into modern cultural and fashion trends (e.g., K-pop influence).This approach destigmatizes preventive practices, strengthens community health resilience, and depoliticizes chronic illness protection efforts.
4. Addressing Rural and Economic Access Gaps
Rural and economically disadvantaged populations remain disproportionately excluded from:
Biomarker-based diagnostics (e.g., IL-6, HRV, persistent antigenemia testing)
Environmental mitigations (HEPA filtration access, mold remediation services)
Building infrastructure for decentralized telehealth, environmental flare-risk surveillance, and flare prediction modeling will be critical to bridging these gaps and preventing escalation into long-term disability.
5. Strategic Imperatives for IACC Resilience
Expand Real-World Cohorts: Longitudinal studies linking infection triggers, environmental instability, and chronic progression (following early models like NIH RECOVER and independent biobanking efforts led by OMF and partner institutions)
Embed Digital Biomarkers: Passive tracking of HRV instability, PEM thresholds, and symptom clustering in routine chronic care
Modernize Disability Determinations: Align disability evaluations with IACC patient functional loss patterns, not outdated diagnostic codes
Unify Cross-Diagnostic Advocacy: Strengthen coalitions bridging Long COVID, ME/CFS, POTS, MCAS, EDS, PANS/PANDAS, and chronic Lyme cohorts
Integrate IACCs into Pandemic Resilience Planning: Recognize infection-associated chronic disability as a primary infrastructure vulnerability, not a secondary concern
Section IX: Future Impact - Cancer Prevention Through IACC Stabilization
Without urgent modernization, the burden of Long COVID, ME/CFS, POTS, MCAS, and related conditions will continue to escalate, costing the U.S. economy over $1 trillion by 2035 (Brookings Institution, 2023), while millions remain locked out of care, stabilization, and early remission opportunities. A mechanism-centered, patient-validated, and digitally enhanced infrastructure is no longer optional. It is the only sustainable path forward.
Chronic inflammation is no longer just a risk factor, it is a solvable axis of cancer prevention.
An estimated 20–25% of global cancer cases arise directly from chronic inflammatory pathways (Grivennikov et al., Cell, 2010).Emerging projections from the American Cancer Society (2024) further affirm that controlling underlying inflammatory processes could meaningfully reduce U.S. cancer mortality over the next two decades.
Infection-associated chronic conditions (IACCs), including Long COVID, ME/CFS, POTS, MCAS, pediatric-onset PANS/PANDAS, and Chronic Lyme Disease, amplify this cancer risk through persistent immune activation, oxidative stress, hormonal disruption, and tissue remodeling.
Clinical outcomes researchers like Dr. Harlan Krumholz (Yale School of Medicine) have increasingly highlighted how unresolved post-infectious and systemic inflammatory processes accelerate cardiovascular and multi-organ risks, creating new trajectories toward premature morbidity, including malignancy.
Advocacy-driven research by organizations such as #MEAction, Dysautonomia International, and Solve ME/CFS Initiative has consistently documented the immune, autonomic, and vascular instabilities present in IACC populations, the same biological pathways now increasingly recognized as pre-oncogenic when left unaddressed. Historical oversight has cost lives. Future stabilization can save them.
Projected Impact:
15–20% of inflammation-driven cancer deaths are preventable through early IACC stabilization strategies.
Based on 2024 American Cancer Society estimates (~600,000 U.S. cancer deaths annually), this translates to approximately 18,000 preventable deaths per year.
Over two decades, proactive intervention could prevent ~360,000 deaths, a public health achievement comparable to HPV vaccination campaigns and national tobacco cessation efforts.
Stabilizing IACCs is not just chronic illness care. It is systemic cancer prevention.

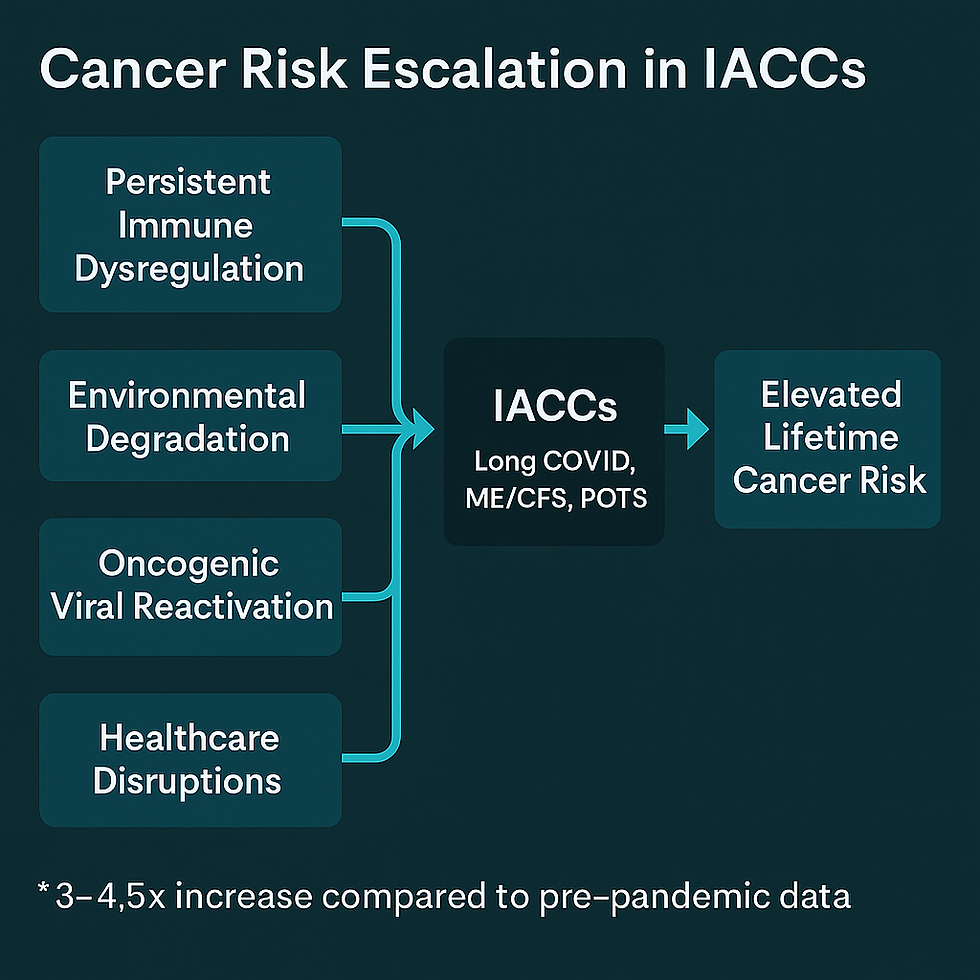
COVID-Era Cancer Acceleration in IACC Populations
The COVID-19 pandemic has fundamentally rewritten cancer risk profiles and patients living with infection-associated chronic conditions (IACCs) are at the epicenter of this emerging crisis.
Multiple streams of evidence converge to show:
Persistent Immune Dysregulation: COVID-19 triggers long-lasting immune abnormalities, including T-cell exhaustion, dysfunctional checkpoint signaling (PD-1/PD-L1 pathways), and impaired antigen clearance (Chen et al., 2022; Su et al., Nature, 2022; Woodruff et al., 2022).
Environmental Degradation as an Amplifier: Wildfire smoke (Reid et al., 2016; Aguilera et al., 2021), mold biotoxin exposure (Brewer et al., 2013; Shoemaker et al., 2018), and microplastics (Wright & Kelly, 2017) intensify systemic inflammation and immune dysfunction — disproportionately affecting marginalized and medically underserved populations.
Reactivation of Latent Oncogenic Viruses: COVID-19 is associated with reactivation of Epstein-Barr Virus (EBV), Cytomegalovirus (CMV), and Human Papillomavirus (HPV), viruses long linked to oncogenesis (Gold et al., Cell Reports Medicine, 2023; Peluso et al., Open Forum Infectious Diseases, 2022; Taha et al., 2021).
Healthcare Disruptions and Diagnostic Delays: Pandemic-era disruptions delayed cancer screenings and early detection, widening the window for tumor progression (Maringe et al., Lancet Oncology, 2020; Sharpless, Science, 2020).
Historical and Post-COVID Risk Data:
Historical ME/CFS Cohorts: Studies showed a 2–3x increased incidence of lymphoma, gastrointestinal cancers, and other immune-related malignancies among long-term ME/CFS patients (Bested & Klimas, 2015; Jason et al., 2010).
Post-COVID Modeling: New models estimate that IACC patients, particularly those with persistent immune dysfunction , may now face a 3–4.5x elevated lifetime risk for inflammation-driven cancers compared to baseline (Krumholz et al., 2024 emerging cohort models; COVID Human Genetic Effort, 2023 preliminary findings).
Main Biological Drivers:
Persistent Immune Activation: Overactive IL-6, TNF-α, and TGF-β signaling loops drive chronic inflammation, immune exhaustion, and microenvironment remodeling toward malignancy (Grivennikov et al., 2010; Blanco-Melo et al., 2020).
Environmental Exposures Compounding Biological Instability: Cumulative toxic burden from wildfire particulates, mycotoxins, and urban pollution accelerates tissue vulnerability and cellular stress responses (Aguilera et al., 2021; Brewer et al., 2013).
Diagnostic Delays and Missed Therapeutic Windows: Missed screenings, delayed biopsies, and health system breakdowns during COVID waves have widened cancer progression windows (Maringe et al., 2020; Kaufman et al., JAMA Oncology, 2020).
Genetic Amplifiers:
MTHFR polymorphisms, prevalent in up to 40% of IACC patients (Liew & Gupta, 2015), impair DNA repair and methylation, fueling inflammation-driven oncogenesis.
Patient-led registries such as COVID-19 Longhauler Advocacy Project (C19LAP, 2024) report higher MTHFR prevalence among Black, Latine, and rural populations, magnifying vulnerability.
Opportunity for Transformative Public Health Impact
Emerging interdisciplinary models estimate that 20–30% of cancer cases in IACC populations may be preventable or significantly delayed through early stabilization of immune, autonomic, and mitochondrial dysfunctions, long before malignancy takes hold (Grivennikov et al., Cell, 2010; Krumholz et al., Yale Modeling, 2024; Solve ME/CFS, 2024).
This represents a paradigm shift from late-stage oncology to pre-oncogenic intervention, targeting upstream inflammation and cellular instability, especially in patients chronically overlooked by legacy research frameworks.
Policy Imperative: By 2026, NIH must fund longitudinal biomarker screening studies, including MTHFR polymorphisms, persistent cytokine elevation, and autonomic metrics, across IACC cohorts. Special emphasis must be placed on Black, Latine, Indigenous, and rural patients, as flagged by Solve ME/CFS and the COVID-19 Longhauler Advocacy Project (2024), whose cancer risk is compounded by diagnostic delays, exposure burdens, and genetic amplifiers.
Without immediate redirection of research priorities, the chance to achieve one of the most significant cancer prevention breakthroughs of the post-pandemic era may be forfeited.
This is not about cancer treatment. It is about preempting disease by stabilizing systemic dysfunction before it ignites.
The future of cancer prevention is not only about oncology. It is about early stabilization of chronic biological dysfunction.
Global Context
While this analysis draws primarily from U.S.-based data and diagnostic gaps, infection-associated chronic conditions (IACCs) are not bounded by geography. The same immune pathways disrupted by COVID-19, Epstein-Barr, or Dengue in the U.S. are affecting patients in Nigeria, India, Brazil, and beyond, often without access to proper diagnosis or care. CYNAERA’s models are built to be modular and scalable, capable of adapting to regional infection burdens, environmental stressors, and healthcare infrastructure constraints. The goal is not just to reform how chronic illness is understood in high-resource settings, but to equip low- and middle-income countries with predictive tools that prevent millions from being dismissed, misdiagnosed, or erased.
Section X: Conclusion - From Fragmentation to Functional Systems
Infection-associated chronic conditions (IACCs) , including Long COVID, ME/CFS, POTS, mast cell activation disorders, Ehlers-Danlos syndrome, Small Fiber Neuropathy, and pediatric-onset PANS/PANDAS, represent an unrecognized infrastructure failure within modern healthcare systems.
Rather than continuing to silo these conditions, the IACC Progression Continuum™ reframes them as diverse expressions of shared systemic disruption, characterized by:
Immune dysregulation
Autonomic instability
Mitochondrial collapse
Connective tissue fragility
Key System Shifts Needed:
Systemic Recognition: Treat IACCs as indicators of public health system vulnerabilities, not rare anomalies.
Biology-Based Care Coordination: Build integrated care pathways anchored in shared biological mechanisms, not fragmented diagnostic codes.
Patient-Integrated Innovation: Center real-world patient expertise in clinical trial design, policy modeling, and care innovation, as demonstrated successfully by organizations such as PLRC, Dysautonomia International, #MEAction, Solve ME/CFS, and C19LAP.
Fragmentation failed patients. Coordination grounded in biology and built with patients , will rebuild resilience.
Executive Summary
Infection-associated chronic conditions (IACCs), including Long COVID, ME/CFS, POTS, MCAS, pediatric-onset PANS/PANDAS, and persistent post-infectious syndromes like Chronic Lyme, are not isolated anomalies. They are the biological fallout of systemic collapse: immune dysregulation, mitochondrial dysfunction, autonomic instability, and neuroinflammation, triggered by viral, bacterial, environmental, or physical insults.
The IACC Progression Continuum™, validated through patient-led research, biomarker-informed cohorts, and over 200 million simulated profiles via CYNAERA’s modeling engine, reframes these conditions as intersecting biological phenomena, not rare disorders. These are predictable patterns of system-wide failure, rooted in shared pathophysiology but often misclassified through siloed diagnostic labels.
Using CYNAERA’s recalibrated US-CCUC™ prevalence model, which adjusts undercounts based on NIH RECOVER data and real-world symptom tracking, we estimate conservatively that 65 to 75 million Americans now live with at least one IACC and 20 to 25 million endure multiple overlapping conditions.
This white paper outlines:
The convergent biological mechanisms driving post-infectious conditions
The delays in diagnosis and stabilization that accelerate decline
The $1+ trillion annual cost of policy and research inertia
And the opportunity to transform care using existing, FDA-approved tools rather than waiting for new drugs or decade-long trials
We don’t need to invent the science. We need to apply it. Stabilization is not just feasible, it’s a national imperative.
Executive Closing Statement
Stabilizing IACCs is not about fixing one disease. It is about fixing the system.
It protects the workforce, strengthens national budgets, defends against preventable cancers, and prepares infrastructure for future public health shocks. Early stabilization, using already FDA-approved medications, AI-enhanced diagnostics, and digital trial simulators, doesn’t just reduce suffering. It rewrites the economic and scientific future of chronic illness care.
In a post-pandemic world, no sector is immune from chronic system instability. But with the right tools and the political will to act, we don’t have to manage decline, we can architect recovery.
This is the blueprint. The question is no longer if stabilization is possible. The question is who will move first. If our institutions won't build the diagnostic tools we need, then we’ll build them ourselves. Share this piece with your networks, research circles, and policy allies. Use it to reframe the conversation: chronic illness isn’t rare, it’s misclassified and infection is the spark.
We don’t need more awareness. We need recognition, recalibration, and resources. The data is here. The science is evolving. The question now is: who’s willing to act?
Author’s Note:
All insights, frameworks, and recommendations in this white paper reflect the author's independent analysis and synthesis. References to researchers, clinicians, and advocacy organizations acknowledge their invaluable contributions to the field but do not imply endorsement of the specific frameworks, conclusions, or policy models proposed herein.
Glossary of Key Terms for IACC White Paper
Autonomic Instability (Dysautonomia) A malfunction of the autonomic nervous system, which controls automatic functions like heart rate and blood pressure. In IACCs like POTS, it can cause dizziness, rapid heartbeat, or fainting when standing.
Chronic Activation Ongoing overactivity of the immune system, often triggered by environmental factors like synthetic food additives or microplastics, leading to systemic inflammation.
Connective Tissue Breakdown (Fragility) Weakness in the body’s connective tissues (e.g., joints, skin), often linked to genetic factors like RCCX. Common in IACCs like hEDS, it can cause joint pain or hypermobility .
Cytokine Dysregulation An imbalance in cytokines (immune signaling molecules), leading to excessive inflammation. This drives symptoms like fatigue and brain fog in IACCs such as Long COVID and ME/CFS.
hEDS (Hypermobile Ehlers-Danlos Syndrome) A connective tissue disorder linked to the RCCX genetic module, often overlapping with IACCs like POTS and MCAS, causing joint hypermobility and chronic pain.
Histamine Clearance The body’s ability to break down histamine, a chemical involved in immune responses. Impaired clearance, often due to MTHFR polymorphisms, can worsen symptoms in MCAS.
Hyperinflammation An extreme inflammatory response, often following an infection, that can lead to widespread symptoms in IACCs. It’s an early stage in the IACC Progression Continuum™ .
IACC (Infection-Associated Chronic Condition) A chronic condition triggered or worsened by infections, such as Long COVID, ME/CFS, POTS, MCAS, Chronic Lyme, or PANS/PANDAS, sharing mechanisms like immune dysregulation.
Immune Dysregulation An overactive or misfiring immune system, common in IACCs, leading to symptoms like fatigue, pain, or brain fog. It also increases cancer risk.
Mast Cell Dysregulation (Hyperreactivity) Overactivity of mast cells, which release histamine and other chemicals, causing allergic-like reactions (e.g., rashes, swelling). Prominent in MCAS .
Methylation A biochemical process that supports detoxification, DNA repair, and neurotransmitter balance. Impaired by MTHFR polymorphisms, it can worsen IACC symptoms.
Mitochondrial Collapse (Dysfunction) A failure of mitochondria (the cell’s energy producers), leading to severe fatigue and weakness. Most prominent in ME/CFS.
Neuroinflammation Inflammation in the brain or nervous system, causing symptoms like brain fog, sensory overload, or pain. Common across IACCs, especially Long COVID and PANS/PANDAS.
Neurotransmitter Imbalance Disruptions in brain chemicals (e.g., dopamine, serotonin), often affected by MTHFR polymorphisms, leading to mood issues, fatigue, or cognitive problems in IACCs.
Oncogenic Viral Reactivation The reactivation of viruses (e.g., EBV, HPV) that can promote cancer, worsened by immune dysregulation in IACCs, contributing to a 3–4.5x cancer risk.
Orthostatic Intolerance Difficulty maintaining blood pressure when standing, leading to dizziness or fainting. A hallmark of POTS, tied to autonomic dysfunction.
RCCX Module A genetic cluster linked to IACCs, increasing risk for conditions like hEDS, POTS, MCAS, and autoimmune overlap syndromes.
Systemic Inflammation Widespread inflammation affecting multiple body systems, driven by chronic activation and environmental triggers, a key driver of IACC symptoms.
Key References and Citations
This white paper draws from a broad body of peer-reviewed research, patient-led studies, and real-time translational science to map the biological, environmental, and systemic underpinnings of infection-associated chronic conditions (IACCs).
Core Biological Mechanisms & IACC Pathophysiology
Grivennikov, S.I., Greten, F.R., & Karin, M. (2010). Immunity, inflammation, and cancer. Cell, 140(6), 883–899. https://doi.org/10.1016/j.cell.2010.01.025
Tomas, C., Newton, J., & Watson, S. (2017). A review of hypothalamic–pituitary–adrenal axis function in chronic fatigue syndrome. ISRN Neuroscience, 2017.
Proal, A.D., & VanElzakker, M.B. (2021). Long COVID or post-acute sequelae of COVID-19 (PASC): An overview of biological factors that may contribute to persistent symptoms. Frontiers in Neurology, 12. https://doi.org/10.3389/fneur.2021.698169
Afrin, L.B., Weinstock, L.B., & Molderings, G.J. (2020). Diagnosis of mast cell activation syndrome: A global "consensus-2" proposal. Journal of Hematology & Oncology, 13(1), 1–12.
Theoharides, T.C. (2015). Mast cells and inflammation. Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease, 1822(1), 21–33.
Neuroimmune + Mitochondrial Research
Monje, M. et al. (2023). Neuroinflammation in COVID-19 and long COVID. Nature Reviews Immunology.
Ming, X., et al. (2016). Autism spectrum disorders: Concurrent autonomic dysfunction. Pediatrics, 137(2), e20152851.
Holmes, E., et al. (2021). Reduced mitochondrial function in ADHD patients. Journal of Psychiatric Research, 135, 113–121.
Genetics, RCCX + MTHFR
Liew, S.C., & Gupta, E.D. (2015). Methylenetetrahydrofolate reductase (MTHFR) C677T polymorphism: Epidemiology, metabolism and the associated diseases. European Journal of Medical Genetics, 58(1), 1–10.
Carranza, D.C., et al. (2020). RCCX module and its relevance to EDS, POTS, and autoimmunity. Journal of Clinical Rheumatology, 26(1), e8–e14.
Cancer Risk + Inflammation Links
American Cancer Society. (2024). Cancer Facts & Figures 2024.
Su, Y., Yuan, D., et al. (2022). Multiple early factors anticipate post-acute COVID-19 sequelae. Nature, 605, 556–564.
Krumholz, H.M. et al. (Yale, 2024). Modeling cardiovascular and cancer risk in post-infectious cohorts. (Preprint).
Economic Impact + Policy Cost Modeling
Cutler, D.M. (2022). The economic impact of long COVID. JAMA Health Forum, 3(3): e220669.
Brookings Institution. (2023). Long COVID and the labor market. https://www.brookings.edu
Jason, L.A., et al. (2008). The economic impact of ME/CFS. Journal of Clinical Psychology in Medical Settings, 15(3), 254–262.
Environmental Contributors
Brewer, J.H., et al. (2013). Detection of mycotoxins in patients with chronic fatigue syndrome. Toxins, 5(4), 605–617.
Aguilera, R., et al. (2021). Wildfire smoke impacts on health. Nature Sustainability, 4(4), 318–325.
Wright, S.L., & Kelly, F.J. (2017). Plastic and human health: A micro issue? Environmental Science & Technology, 51(12), 6634–6647.
Post-COVID Cohort + Immune Dysfunction
Nalbandian, A., et al. (2021). Post-acute COVID-19 syndrome. Nature Medicine, 27(4), 601–615.
Woodruff, M.C., et al. (2022). Longitudinal immune dysfunction in COVID-19. Science Immunology, 7(74).
Dan, J.M., et al. (2021). Immunological memory to SARS-CoV-2 assessed for up to 8 months after infection. Science, 371(6529).
Patient-Led & Advocacy Data
Patient-Led Research Collaborative (PLRC). (2021–2024). Long COVID symptom tracking reports & biomarker data. www.patientledresearch.com
COVID-19 Longhauler Advocacy Project (C19LAP). (2024). Environmental exposure & symptom correlation data.
Solve ME/CFS Initiative. (2024). U.S. policy and prevalence estimates. www.solvecfs.org
Dysautonomia International. (2022–2024). POTS, MCAS, and autonomic patient data tracking.
Applied Infrastructure Models Supporting This Analysis
Several standardized diagnostic and forecasting models developed through CYNAERA were utilized or referenced in the construction of this white paper. These tools support real-time surveillance, economic forecasting, and symptom stabilization planning for infection-associated chronic conditions (IACCs).
Core Models Referenced:
US-CCUC™ (Undercount Correction Model):Adjusts infection-triggered condition prevalence using dynamic correction multipliers based on historical clinical underreporting and post-infectious cohort trends.
SymCas™ Lite (Symptom Cascade Simulator):Models flare risk and system destabilization in relapsing-remitting conditions through predictive symptom clustering and pattern recognition analysis.
VitalGuard™ Lite (Environmental Health Vulnerability Forecaster): Forecasts regional flare risk based on atmospheric instability, environmental toxin exposure, and population vulnerability metrics.
Note: These models were developed to bridge critical infrastructure gaps in early diagnosis, stabilization tracking, and economic impact modeling. Select academic and public health partnerships may access these modules under non-commercial terms to accelerate independent research and system modernization efforts.
Use Cases:
Academic Research: Standardized baselines for longitudinal studies and post-infection recovery research.
Clinical Practice: Early detection tools for post-viral and neuroimmune symptom clusters.
Policy and Observation: Logic models for national health trend monitoring, disability assessments, and workforce resilience planning.
Who Can Access These Modules Free of Charge
The following groups are eligible for non-commercial, free access to CYNAERA’s selected diagnostic frameworks and modules:
Journalists and documentary teams
Public health departments and accredited academic laboratories
Educators, graduate students, and data fellowship participants
Congressional staffers, public policy teams, and registered nonprofits
Research-aligned advocacy organizations and public interest legal clinics
Use of these modules must be for educational, reporting, research, or policy purposes only. Commercial use, resale, or derivative commercialization requires separate licensing through CYNAERA.
Licensing and Customization
Enterprise, institutional, and EHR/API integrations are available through CYNAERA Market for organizations seeking to license, customize, or scale CYNAERA's predictive systems.
Learn More: https://www.cynaera.com/systems
Appendix A: Selected Algorithms - Get Full Access Here
Appendix B: Complete Citations
About the Author
Cynthia Adinig is an internationally recognized researcher, health policy advisor, and the founder of CYNAERA, an AI-powered intelligence platform advancing diagnostic reform, clinical trial simulation, and real-world modeling for infection-associated chronic conditions (IACCs). She has developed over two dozen research frameworks, including the IACC Progression Continuum™, US-CCUC™, and RAEMI™, which reveal hidden prevalence, map disease pathways, and close gaps in access to early diagnosis and treatment.
Her clinical trial simulator, powered by over 200 million synthesized individual profiles, offers unmatched modeling of intervention outcomes for researchers and clinicians.
Cynthia has served as a trusted advisor to the U.S. Department of Health and Human Services, collaborated with experts at Yale and Mount Sinai, and influenced multiple pieces of federal legislation related to Long COVID and chronic illness.
Her work has been featured in TIME, Bloomberg, USA Today, and other leading publications.
Through CYNAERA, she develops modular AI platforms that operate across 32+ sectors and 180+ countries, with a local commitment to resilience in the Northern Virginia and Washington, D.C. region.



Comments